Cleft lip/palate multidisciplinary program is design to give general guidelines of medical intervention and management for patients with cleft lip/Palate. This program is flexible and intended to be suitable for the majority of the patients.
Scope (goal):
The main goal of cleft lip and palate program is to determine the composition of interdisciplinary team and their responsibilities and develop a treatment plan through evaluation, management, rehabilitation and counseling, and provide educational martial to patient, caregiver and their families
Organization of the Guidelines:
The guidelines represent the minimum requirements in caring for individuals with cleft lip and/or palate. Care of treatment should be consistent throughout the program, therefore the involved teams need to adhere to the guidelines after its approval and the suggested organizing structure is as follow.
Multidisciplinary Team Membership:
The following team member will be available to review patient in clinic and be available for inpatient consultation or coordinate care with inpatient staff. It may be not necessary for each member to see the patient at each visit. One team member can fill more than one role if properly trained.
The multidisciplinary team consists of:
- General pediatrician
- Cleft lip and palate Nurse Coordinator
- Medical Geneticist
- Orthodontist
- Oral and Maxillofacial surgeon.
- Otolaryngologist
- Plastic surgeon
- Speech therapies
- Other specialties: Dietician .Psychological and Social Services will be utilized, at the first phase of the program, as case per case consultation.
Team/Staff Meeting:
- Evaluate patient at the first phase of the program, Discussion of findings, treatment planning, and recommendations for each patient. And meetings will be per requirement and dependent on patient case.
- Develop the treatment plan for each patient that is modified as necessitated by treatment outcome and therapeutic advances
- Communicate the treatment recommendation for each patient and update the progression.
- Such meeting frequency and timing will be determined later after evaluating the success of the team care and the needs or such meetings.
Team responsibilities
General Pediatrician:
- Pediatrician will assess for all common pediatric issue including nutrition, growth and development, psychosocial issue and immunization.
- When special needs are identified, referral to appropriate specialists will be arranged.
- Frequent monitoring is required for children who may be at risk for growth failure, delayed development, neglect, psychosocial disturbance or any other significant problem.
- The child’s health status will be evaluated prior to any surgical procedures that are planned and discussed with team if needed.
- The optimal time for the first visit is at six week of live. The second visit at three month of age then will at six month and 12 month of age. In case any medical issue pediatrician will give appointment depend on that issue.
Cleft Lip and Cleft Palate Program Nurse Coordinator (CLCPPNC):
The principle role of coordination is to facilitate the function of the team and provide care and support for patient and family. The responsibility of coordinator as following:
General Duties:
- Coordinate the activity of the multidisciplinary team and facilitate the patient care.
- Ensure patients medical and psychological issues are addressed
- Maintain supporting for the family through telephone calls or visiting nurse clinic.
- Provide instruction and educational materials about feeding and provide other information such as the availability of special feeding devices.
- Ensue frequent assessment of nutritional intake and weight gain and growth assessment
- Prepare patient and family about what expect when surgical procedure are schedule. Information should include pre and postoperative feeding, wound care and daily activity.
Detailed management:
- Meet family, obtain medical history and introduce the program.
- Explain to family/caregiver beyond the abnormality, there are other possible complications that may be associated with cleft lip and/or palate, including the following:
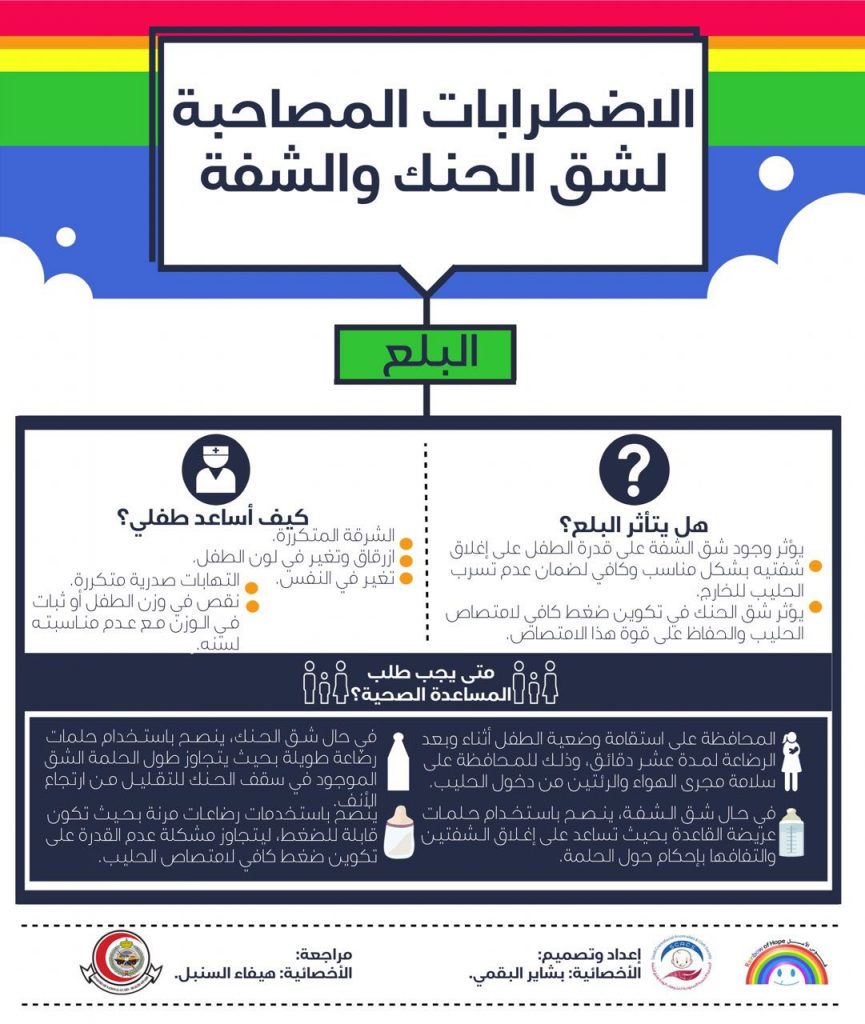
- Feeding difficulties
Feeding difficulties occur more with cleft palate abnormalities. The infant may be unable to suck properly because the roof of the mouth is not formed completely.
- Ear infections and hearing loss
Ear infections are often due to a dysfunction of the tube that connects the middle ear and the throat. Recurrent infections can then lead to hearing loss.
- Speech and language delay
Due to the opening of the roof of the mouth and the lip, muscle function may be decreased, which can lead to a delay in speech or abnormal speech.
- Dental problems
As a result of the abnormalities, teeth may not erupt normally and orthodontic treatment is usually required.
- Teach parent how to feed their infant and make sure they are able to provide an effective, satisfying and nutritious feeding for their infant.
- Monitor the child’s development throughout the first year of life height, weight gain, nutrition, feeding and appropriate calorie intake, and immunizations.
- Ensure weekly assessment of nutritional intake and weight gain during first 2 months of life and will be frequent assessment and depend on condition.
- Coordinate the evaluation by different team and ensure appropriate care is provided.
- Book patients in various specialties and ensure they come on time.
- Prepare patient and family for any procedures and provide pre and postoperative care and instructions.
- Arrange for farther evaluation by non-multidisciplinary team like swallowing, and ophthalmological evaluation as needed.
Medical Geneticist:
- All patients need to be evaluated by collecting medical information including family history and physical examination looking for associated genetic syndrome or related hereditary disorder.
- Parents and adult patients will receive detailed genetic Counseling and review recurrence risks.
- Patients should be seen at least once in infancy, preferably in the neonatal period and the second visit at 5-6 years of age while the last visit is post-adolescent or premarital period
Oral and Maxillofacial surgeon:
Some infants born with cleft lip and/or palate may have other craniofacial anomalies. The complex nature of many types of craniofacial anomalies often necessitates multiple operative procedures at different stages of development. Follow-up is necessary for these patients even when the intervention has been successful.
The general roles are:
- Pre-surgical use of a dental plate (Latham appliance) to align the maxillary segments prior to initial lip and palate repair (from birth).
- Initial evaluation, physical examination, and timing of surgery for patients cranial vault anomalies and orbitocranial anomalies, including abnormalities of orbital position and shape and globe position should be performed as needed.
- Secondary procedures to correct residual deformities of the mandible, maxilla, orbits, zygoma, forehead, and nose as necessary.
- Orthognathic surgery (and/or distraction osteogenesis) is indicated when orthodontic treatment cannot achieve functional and/or acceptable aesthetic occlusion and facial harmony. orthognathic surgery should be delayed until physical maturation is essentially completed. Earlier surgery may be indicated when there is compromised airway, jaw function, speech, or psychosocial adjustment.
- If mandibular ankylosis is present, surgical release should be considered as soon as the condition is diagnosed. Both surgical intervention and subsequent physical therapy may be necessary to facilitate mandibular development
Orthodontist:
Patients with cleft lip and/or palate require dental services for monitoring craniofacial growth and development, monitoring healthy dentition, correcting jaw and dental occlusion in order to achieve optimal function and appearance:
- Align the maxillary dentition (usually using fixed appliances) in the growing child if the appearance causes the child distress or the irregular teeth are traumatizing soft tissues (6+ years).
- Preparation for alveolar bone grafting (7+ years)
- Align maxillary and mandibular teeth in the teenager using fixed appliances (12+ years).
- Prepare for orthognathic surgery using fixed appliances and to detail the occlusion post-operatively.
- Fabrication of palatal lift appliances for patients with velopharyngeal dysfunction.
Detail Management:
- Dental radiographs, cephalometric radiographs, and other imaging modalities as inducted.
- Diagnostic records, including properly occluded dental study models, should be collected at appropriate intervals for patients at risk for developing malocclusion or maxillary mandibular discrepancies
- Presurgical maxillary orthopedics to improve the position of the maxillary alveolar segments prior to surgical closure of the lip may be indicated for some infants.
- As the primary dentition erupts, the team evaluation should include a dental examination and preventive measures.
- Before the primary dentition has completed eruption, the skeletal and dental components should be evaluated to determine if a malocclusion is present or developing.
- Congenitally missing teeth may be replaced with a removable appliance, fixed restorative bridgework, or osseointegrated implants.
- Prosthetic obturation of palatal fistulae may be necessary in some patients. A prosthetic speech device may be used to treat velopharyngeal inadequacy in some patients
Otolaryngologist and Audiologist:
Infants born with a cleft palate have recurrent middle ear fluid and may develop an ear disease that is related to failure of the ventilatory function of the Eustachian tube. Eustachian tube dysfunction causes Otitis Media with Effusion (OME), commonly known as glue ear. This is associated with a high incidence of acute otitis media due to secondary infection, tympanic membrane abnormalities including perforations and cholesteatoma. On the other hand, craniofacial anomalies may have congenital abnormalities of the auditory structures and are also subject to an increased incidence of ear disease.
The following are the otolaryngologist roles in case with cleft palate:
- Physical examination of the ears.
- Usually follow-up every six months of all primary school aged children with cleft palate.
- In the absence of a positive history of otologic disease or hearing loss, audiologic examination or screening should still be carried out at least yearly through the age of six years to assure adequate monitoring of hearing.
- Acoustic-immittance emission (except for cleft palate) and tympanometry measures should be obtained as a part of each audiological evaluation to monitor middle ear status.
- All children undergoing myringotomies and placement of ventilating tubes will be seen pre- and postoperatively for audiologic assessment to ensure a successful outcome
- The management of secretary otitis media (SOM) involves the use of ventilation tubes inserted through the tympanic membrane under general anesthesia.
- When a persistent hearing loss is identified, amplification (hearing aids, auditory training systems) should be considered.
- Once amplification has been provided, a regular follow-up schedule is needed to monitor hearing thresholds and the function of the amplification system.
- assessment of the velopharyngeal mechanism prior to any decision to perform such a procedure.
Plastic surgery:
In addition to surgical closure of the lip and palate, patients may require another surgical procedures involving the lip, nose, palate, and jaws. These procedures usually are staged over a period of several years. In all cases, surgery should be individualized according to the needs and condition of the patient:
- The goal of lip repair is to restore the normal functional and anatomic features. Surgical repair of the cleft lip is usually done at age of 3-6 months of life and may be performed as early as is considered safe for the infant.
- The nasal deformity is an integral part of the cleft lip. Depending on the severity, rhinoplasty may be done at the time of the primary lip repair.
- The goal of palate surgery is to achieve normal function; the palate will be closed by the age of 12 -18 months.
- Velopharyngeal inadequacy(VPI) will be assessed by speech therapist first then referred to plastic if need surgery and can be performed at age of 5 to 6 year
- Surgical or prosthetic closure of palatal fistulae may be needed if the fistulae are symptomatic.
- The timing of bone grafting of the alveolar cleft will be performed at 9-12 year of age when permanent erupt
- Secondary rhinoplasty and nasal septal surgery are indicated only after completion of nasal growth, airway problems or nasal tip deformity and can be performed at 16 to 18 year of age.
Detailed management:
Cleft lip and palate can present with considerable variation in severity and form. These cleft, present a significant surgical challenge to achieve a functional and cosmetic outcome.
- Cleft lip surgery
Cleft lips can range in severity from a slight indent in the lip to a complete separation of the lip extending to the nose. Clefts can occur on one or both sides of the upper lip. Surgery is generally done when a child is 3 to 6 month old. Surgical and recovery time depend on the severity of the defect. In general, after the surgery, the doctor will prescribe medication to relieve discomfort. Usually this is only needed for a couple of days.
- Cleft palate surgery
Cleft palates may only involve a small portion of the back palate, or it may involve the whole roof of the mouth from back to front. Depending on the severity of the defect, surgery may be extensive and is usually not done on children until they are 12 to 18 months old. After the surgery, the child is usually placed on intravenous fluids during hospitalization for a few days to maintain fluid levels and discomfort is controlled by medication.
- Velopharyngeal Inadequancy (VPI)
Speech problems are usually treated by a speech therapy. In some cases pharyngeal flap surgery is performed to regulate the airflow during speech and reduce nasal sounds and it is common used to restore velopharyngeal competency i.e. develop a functional seal between the nasal cavity and the oral cavity, and therefore correct hypernastily and nasal air escape.
- Bone grafting
Bone grafting the dental ridge of the upper jaw is a procedure that may be performed by taking small amounts of bone from elsewhere on the body, such as the hip, ribs, head, or leg, surgeons can reconstruct the area of the cleft near the teeth. The bone graft allows for the formation of a continuous upper gum, supporting the teeth, lip, and nose, and improving facial symmetry and stability. This procedure is often performed at age 9 to 12 year old.
Speech therapist
Children born with a cleft involving the palate are at risk of developing abnormal speech patterns. There is considerable variation in the literature about the number of children with cleft lip and/or palate who go on to have speech problems following primary repair of the palate.
Witzel48 reported that 25% of people with cleft palate developed normal speech spontaneously and 75% required episodes of speech therapy throughout childhood and adolescence. The CSAG1 study audited outcomes of 457 children aged 5 or 12 years who had been treated for unilateral cleft lip and palate in the UK. Approximately 33% of 5 year olds and 14% of 12 year olds presented with serious consonant articulation errors.
Following primary palate repair, cleft speech characteristics that are structural in nature are hypernasality, nasal emission and nasal turbulence. These are all features of resonance and occur when the velopharyngeal sphincter does not close adequately, allowing air to escape into the nose during speech:
- General considerations
- After the age of four years, even if speech-language development has been appropriate and no problems are noted, screenings should take place on a regular basis until after adenoid involution, and at least every three years until dental and skeletal maturity are reached.
- For children with problems in speech and language development, reevaluations should take place as often as necessary.
- Evaluations include perceptual assessment of laryngeal function.
- When the development of speech and language skills is not at an age-appropriate level or when speech patterns are deviant, arrangements should be made for an early speech-language stimulation program
- Pre- and post-treatment speech assessments are necessary in determining candidacy for, and outcomes of, surgical, behavioral and/or prosthetic management of the velopharyngeal system.
- Age related speech and language evaluation
- Birth until palate repair
Support and information to parents about the development of communication and how the cleft may affect speech development. Encouraging normal patterns of parent child interaction.
- Palate repair to 3 years
Monitoring general communication development and advising parents as appropriate, particularly in relation to emerging babble patterns. At 18 months children will have a routine assessment which looks at play skills, social development and interaction, receptive language, expressive language and consonant production.
- 3 years to 5 years
Continued monitoring of all aspects of communication with particular regard to velopharyngeal function and consonant production. At 3 years the child will have more formal assessment of receptive and expressive language skills and an audio and video recorded sample of speech that is analysed in detail.
- 5 years to 10 years
Monitoring and intervention as required based on comprehensively analysed speech sound data.
- 10 and 18 year
Collection and analysis of speech data using audio and video recordings if applicable .
- Velopharyngeal insufficiency
The specialist Speech Therapist with the cleft team will contribute to assessment, diagnosis and treatment planning for children requiring further surgery for velopharyngeal insufficiency affecting speech outcome and symptomatic palatal fistulae. In addition, assessment is required for older children and adults who require maxillary advancement and those needing prosthetic management of velopharyngeal insufficiency where surgery is contraindicated. Speech therapy Intervention can take place at any time but should be appropriate time.
Other specialties
Dietary and psychosocial evaluation is necessary at different stage of patient medical care. Therefore consultation with related specially will be arranges on required bases at the beginning until they are ultimately part of the multidisciplinary team
Psychological and Social Services
The accomplishment of the goals of treatment cleft lip and/or palate require assessment of the psychosocial needs for both patient and family. Psychosocial screening interviews provide management skills, parent-child relationships and emotional and behavioral adjustment of the child.
- Providing guidance regarding such problem as behavior management, public attitude, expectation from surgical procedures and emotional adaptation to treatment.
- Screening evaluation to identify possible problem in the child’s cognitive development, behavior, self concept, educational progress and psychosocial development. It will be conducted beginning in infancy and continuing through adolescence.
- Social skills training to help children and adolescents learn how to handle stressful social situation.
A Psychological and social screening will be performed for parents and the child at regular period starting from the neonatal period by using stander validated screening questionnaires.
Practical consideration during neonatal period and infancy
Inpatient
Evaluation of new inpatient case with cleft lip and/or palate will be within the first few days of life probably within 24 hours after birth.. The program leader or the CLCPP nurse coordinator should be contact first. Upon arrive, the coordinator will assess and perform the following tasks:
- Obtain a history of pre and postnatal period.
- Evaluate the patient and assess his/her associated medical problem.
- Provide a full pediatric evaluation including nutritional and feeding assessments.
- Meet family, collect family history and introduce the program.
- Coordinate and arrange inpatient and out patient care and follow up after discharge.
Outpatient
- If patient is seen previously as inpatient the CLCPP nurse coordinator will follow up the inpatient recommendation and plan and ensure rest of the team evaluates the patient. The coordinator will document all recommendation and discuss with team leader and arrange meeting if necessary.
- If patient was not seen previously, he/she will go for similar inpatient assessment.
- For such plan to be successful and run smoothly all newly accepted outpatients cases are forwarded to the nurse coordinator to facilitate the clinic booking and ensure the medical problems including feedings issues are covered. The notification should be at the time of accepting the patient while signing up the legibility and accepting letter.